Welcome to our dental blog, where we delve into the critical connection between gum disease and diabetes. These two prevalent health issues are more closely intertwined than many realize, with each condition having a significant impact on the other. Understanding this relationship is essential for effective prevention and management of both diseases. In this blog, we will explore how diabetes increases the risk of gum disease, how untreated gum disease can complicate diabetes management, and what steps can be taken to maintain optimal oral and overall health. Join us as we uncover the vital links between these conditions and provide valuable insights for maintaining a healthy smile and a healthy body.
In This Blog:
- Defining Gum Disease and Diabetes
- The Bidirectional Relationship Between Diabetes and Gum Disease
- Preventive Measures for Diabetics
- Treatment Options for Gum Disease in Diabetics
Defining Gum Disease and Diabetes
To fully understand the connection between gum disease and diabetes, it’s important to first define these two conditions and their primary characteristics.
What is Gum Disease?
Gum disease, also known as periodontal disease, is a bacterial infection that affects the gums and the structures that support the teeth. It progresses in stages:
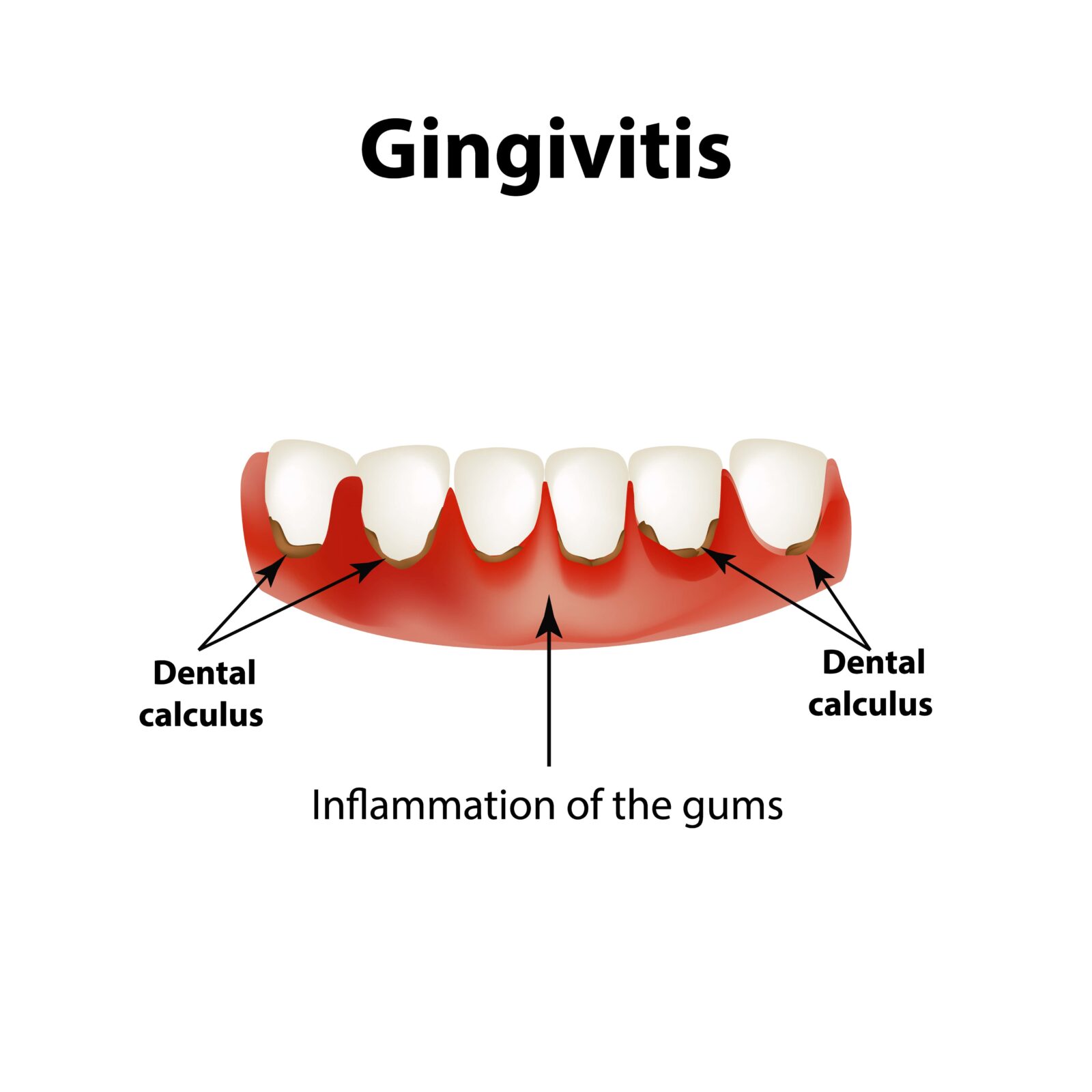
- Gingivitis: This is the earliest stage of gum disease, characterized by red, swollen gums that may bleed easily during brushing or flossing. Gingivitis is caused by plaque buildup on the teeth, which irritates the gums. At this stage, the damage is usually reversible with good oral hygiene and professional dental care.
- Periodontitis: If left untreated, gingivitis can progress to periodontitis, a more severe form of gum disease. In periodontitis, the inner layer of the gum and bone pull away from the teeth and form pockets. These pockets collect debris and can become infected. The body’s immune system fights the bacteria as the plaque spreads and grows below the gum line. Toxins produced by the bacteria, along with the body’s response to the infection, start to break down the bone and connective tissue that hold teeth in place. Without treatment, the bones, gums, and tissue that support the teeth are destroyed, and the teeth may eventually become loose and need to be removed.
Gum disease symptoms can include:
- Red, swollen, or tender gums
- Bleeding gums during brushing or flossing
- Persistent bad breath or bad taste in the mouth
- Receding gums or longer-appearing teeth
- Formation of deep pockets between teeth and gums
- Loose or shifting teeth
What is Diabetes?
Diabetes is a chronic medical condition that affects how the body processes blood sugar (glucose). Glucose is a crucial source of energy for the body’s cells, and insulin, a hormone produced by the pancreas, helps glucose enter the cells. There are several types of diabetes, but the most common are:
- Type 1 Diabetes: This is an autoimmune condition where the body’s immune system attacks and destroys the insulin-producing cells in the pancreas. As a result, the body produces little or no insulin. Type 1 diabetes is typically diagnosed in children and young adults, and those affected require daily insulin injections to manage their blood sugar levels.
- Type 2 Diabetes: This is the most common form of diabetes, where the body either resists the effects of insulin or doesn’t produce enough insulin to maintain normal glucose levels. It is often associated with obesity and tends to develop in adults, although it is increasingly being diagnosed in younger populations. Type 2 diabetes can be managed with lifestyle changes, oral medications, and sometimes insulin.
- Gestational Diabetes: This type occurs during pregnancy and typically goes away after the baby is born. However, women who have had gestational diabetes are at higher risk of developing type 2 diabetes later in life.
Diabetes symptoms can include:
- Increased thirst and frequent urination
- Extreme hunger
- Unexplained weight loss
- Fatigue
- Blurred vision
- Slow-healing sores or frequent infections
The Bidirectional Relationship Between Diabetes and Gum Disease
Understanding the relationship between diabetes and gum disease begins with recognizing how each condition affects the other. Diabetes, characterized by high blood sugar levels, can lead to various health complications, including a higher susceptibility to infections. Gum disease, or periodontal disease, is a bacterial infection that affects the gums and supporting structures of the teeth. Let’s explore how diabetes influences gum health and vice versa.
How Diabetes Affects Gum Health
Individuals with diabetes are at a higher risk of developing gum disease due to several factors:

- Increased Infection Risk: Elevated blood sugar levels impair the body’s immune response, making it harder to fight off bacterial infections, including those in the mouth. This leads to an increased risk of gum disease.
- Poor Blood Flow: Diabetes can cause blood vessels to thicken, reducing the flow of nutrients and oxygen to the gums. This weakened blood supply can slow down the healing process and make the gums more vulnerable to infection.
- High Glucose Levels in Saliva: High blood sugar levels result in higher glucose levels in saliva, creating a favorable environment for harmful bacteria. These bacteria can form plaque, a sticky film that, if not removed, hardens into tartar and irritates the gums.
- Inflammation: Chronic inflammation is a hallmark of diabetes and can exacerbate gum disease. The inflammation damages the tissues and bone that support the teeth, leading to more severe periodontal issues.
The Impact of Gum Disease on Diabetes Management
Gum disease can also negatively impact diabetes management:
- Blood Sugar Control: Gum disease can cause chronic inflammation, which interferes with the body’s ability to utilize insulin effectively. This can lead to higher blood sugar levels, making diabetes more difficult to manage.
- Stress Hormones: Infections, including those from gum disease, cause the body to release stress hormones like cortisol. These hormones can raise blood sugar levels, complicating diabetes control.
- Systemic Inflammation: Gum disease causes inflammation that can spread throughout the body, potentially worsening other diabetes-related complications such as heart disease and kidney damage.
Preventive Measures for Diabetics
Preventing gum disease is crucial for individuals with diabetes. Here are some essential strategies:
Maintain Good Oral Hygiene:
- Brush your teeth at least twice a day with fluoride toothpaste.
- Floss daily to remove plaque between teeth and along the gum line.
- Use an antimicrobial mouthwash to reduce bacteria.
Regular Dental Visits:
- Schedule dental check-ups and professional cleanings every six months.
- Inform your dentist about your diabetes to ensure tailored care.
Control Blood Sugar Levels:
- Monitor your blood sugar levels regularly.
- Follow your diabetes management plan, including diet, exercise, and medications.
Healthy Lifestyle Choices:
- Eat a balanced diet rich in vitamins and minerals that support oral health.
- Quit smoking, as it increases the risk of gum disease.
- Stay hydrated to help wash away food particles and bacteria.
Treatment Options for Gum Disease in Diabetics
If gum disease develops, effective treatment is crucial for managing both oral and overall health:
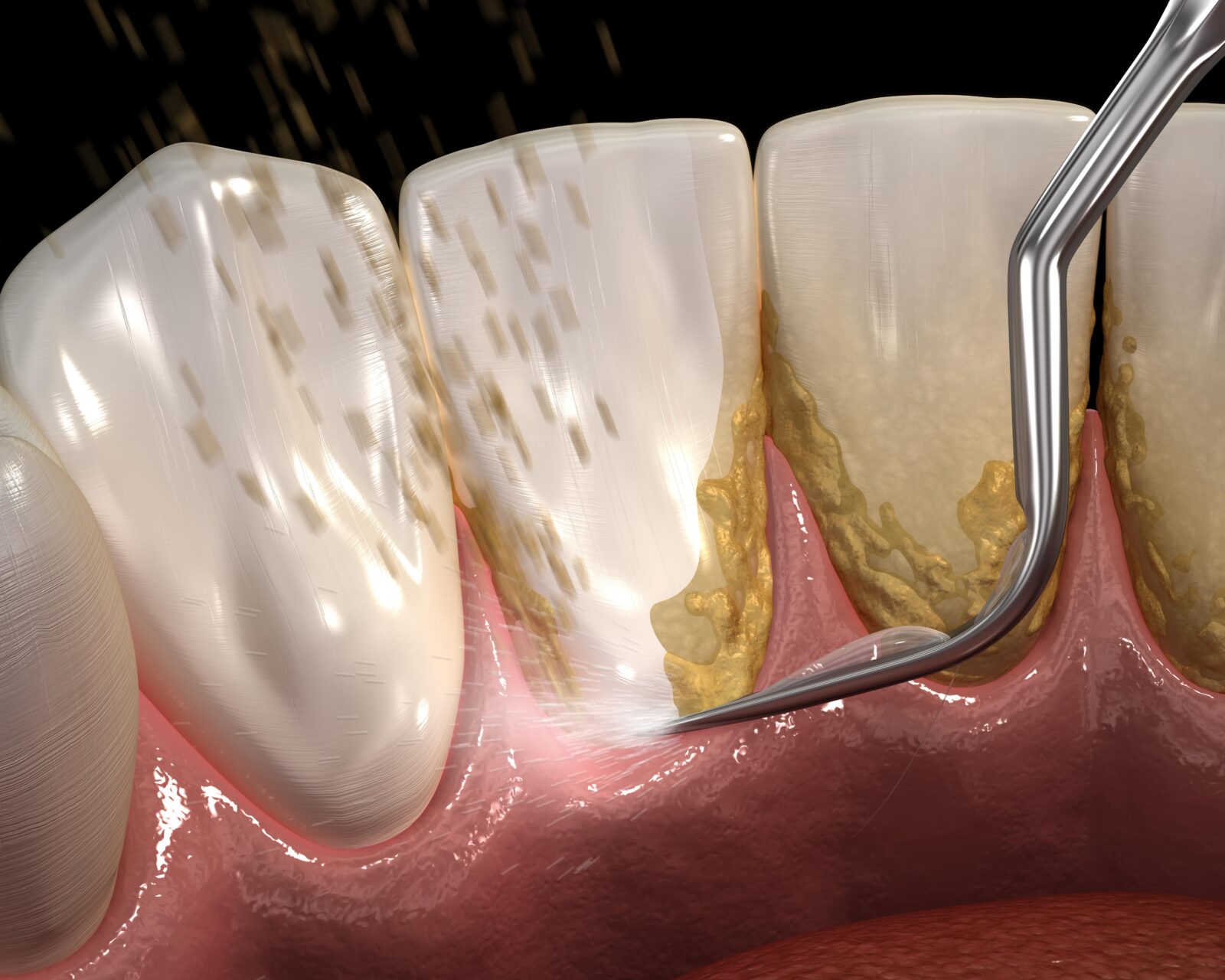
Scaling and Root Planing:
This deep cleaning procedure removes plaque and tartar from below the gum line and smooths the tooth roots, helping gums reattach to the teeth.
Antibiotic Therapy:
Topical or oral antibiotics can be used to control bacterial infection and reduce inflammation.
Periodontal Surgery:
In advanced cases, surgical procedures such as flap surgery or bone and tissue grafts may be necessary to restore damaged gum and bone tissue.
Laser Therapy:
Lasers can remove diseased tissue and kill bacteria in periodontal pockets, promoting healing with minimal discomfort.
Regular Monitoring:
Close collaboration between your dentist and healthcare provider is essential to monitor and manage both diabetes and gum health effectively.
Conclusion
The intricate relationship between diabetes and gum disease highlights the importance of integrated health management. By maintaining good oral hygiene, attending regular dental visits, and managing blood sugar levels, individuals with diabetes can significantly reduce their risk of gum disease and improve their overall health. Understanding and addressing this connection can lead to better health outcomes and a brighter, healthier smile. Stay proactive, stay informed, and take the necessary steps to protect your oral and overall health.